Introduction
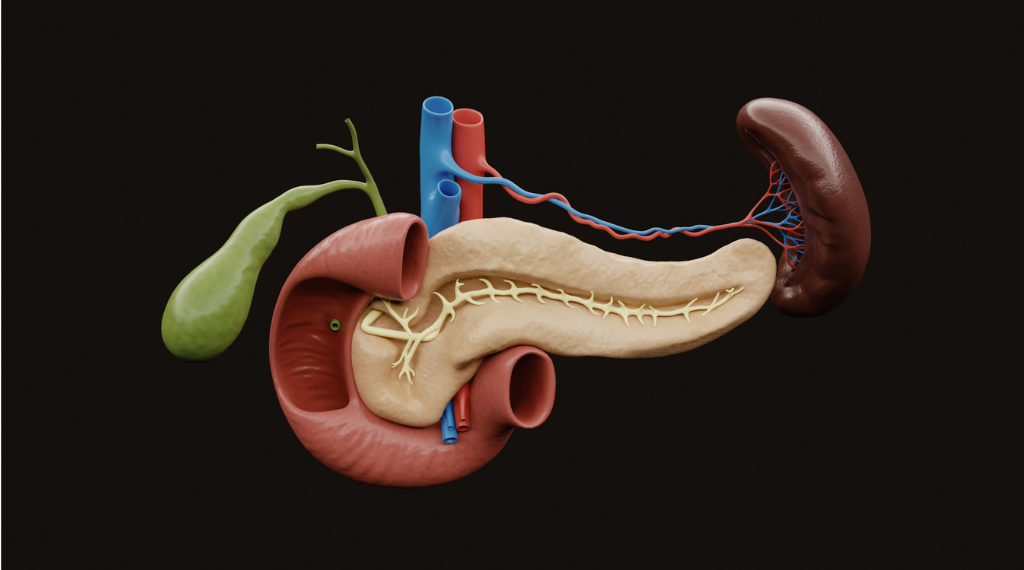
The pancreas is a vital organ that often goes unnoticed until something goes wrong. Tucked behind the stomach, this gland plays a crucial role in both digestion and blood sugar regulation by producing enzymes that break down food and hormones like insulin that control glucose levels. When the pancreas becomes inflamed, damaged, or diseased, the consequences can be severe and potentially life-threatening.
Pancreatic problems are increasingly common, yet many people remain unaware of the warning signs until significant damage has occurred. Early detection is critical because conditions like pancreatitis, pancreatic cancer, and pancreatic insufficiency are far more manageable when caught in their initial stages. Understanding the warning signs your pancreas sends can mean the difference between a manageable health issue and a serious medical crisis.
Causes and Risk Factors
Several factors can compromise pancreatic health, with some being within our control and others predetermined by genetics or circumstance.
Lifestyle Factors: Chronic alcohol consumption is one of the leading causes of pancreatic damage, responsible for approximately 70% of chronic pancreatitis cases. Heavy drinking causes repeated inflammation that eventually leads to permanent scarring. Smoking doubles the risk of pancreatic cancer and accelerates the progression of chronic pancreatitis. A diet high in processed foods, saturated fats, and refined sugars can also strain the pancreas and contribute to inflammation.
Medical Conditions: Gallstones are the most common cause of acute pancreatitis, as they can block the pancreatic duct and trap digestive enzymes inside the organ. High triglyceride levels (above 1,000 mg/dL) can trigger acute inflammation. Diabetes and obesity create metabolic stress that affects pancreatic function over time. Autoimmune disorders can cause the immune system to mistakenly attack pancreatic tissue.
Genetic and Other Factors: Some people inherit genetic mutations that increase their susceptibility to pancreatic diseases. A family history of pancreatic cancer or chronic pancreatitis raises individual risk significantly. Certain medications, abdominal injuries, infections, and anatomical abnormalities of the pancreatic duct can also lead to pancreatic problems. Age is another factor, with pancreatic cancer risk increasing substantially after age 65.

Symptoms: Five Critical Warning Signs
1. Persistent Upper Abdominal Pain
The most common warning sign of pancreatic distress is pain in the upper abdomen that may radiate to the back. This pain often feels like a deep, constant ache rather than sharp cramping. It typically worsens after eating, especially after consuming fatty foods, and may be partially relieved by leaning forward or sitting upright. The pain can last for hours or even days and may become progressively more severe over time.
2. Unexplained Weight Loss and Loss of Appetite
When the pancreas cannot produce adequate digestive enzymes, the body struggles to absorb nutrients from food, leading to weight loss despite normal eating habits. This is often accompanied by a persistent lack of appetite or feeling full quickly after eating small amounts. The weight loss is typically rapid and unintentional, which distinguishes it from deliberate dietary changes. This symptom is particularly concerning when combined with other signs, as it may indicate pancreatic insufficiency or, in more serious cases, pancreatic cancer.
3. Digestive Issues and Changes in Stool
Pancreatic problems frequently manifest as digestive disturbances. People may experience chronic diarrhea, nausea, or vomiting. A telltale sign of pancreatic insufficiency is steatorrhea—pale, greasy, foul-smelling stools that float and are difficult to flush. This occurs because undigested fats pass through the digestive system when pancreatic enzymes are insufficient. Bloating and excessive gas after meals are also common complaints.
4. Jaundice (Yellowing of Skin and Eyes)
When a tumor, inflammation, or stone blocks the bile duct where it passes through the pancreas, bile builds up in the bloodstream, causing jaundice. The skin and whites of the eyes take on a yellowish tint, and urine may appear dark brown while stools become pale or clay-colored. Jaundice accompanied by abdominal pain is a medical emergency requiring immediate evaluation, as it may indicate a blocked duct or pancreatic cancer.
5. New-Onset Diabetes or Difficulty Controlling Blood Sugar
The pancreas produces insulin, so damage to this organ can impair blood sugar regulation. Sudden onset of diabetes in adults, particularly those over 50 without typical risk factors, can be an early warning sign of pancreatic cancer. Even in people with existing diabetes, sudden difficulty controlling blood sugar levels despite no changes in medication or lifestyle may indicate declining pancreatic function.
Treatment and Prevention
Medical Treatments: Treatment for pancreatic conditions varies depending on the underlying cause and severity. Acute pancreatitis typically requires hospitalization with intravenous fluids, pain management, and bowel rest (temporary cessation of eating). Chronic pancreatitis may require pancreatic enzyme replacement therapy to aid digestion, along with pain management strategies. Gallstone-related pancreatitis often necessitates surgical removal of the gallbladder. For pancreatic cancer, treatment options include surgery, chemotherapy, radiation therapy, or a combination approach. Insulin therapy becomes necessary when the pancreas can no longer regulate blood sugar effectively.
Natural and Supportive Remedies: While medical intervention is essential for serious pancreatic conditions, certain natural approaches can support pancreatic health and recovery. An anti-inflammatory diet rich in fruits, vegetables, whole grains, and lean proteins can reduce pancreatic stress. Antioxidant-rich foods like berries, leafy greens, and turmeric may help combat inflammation. Some studies suggest omega-3 fatty acids from fish or flaxseed may have protective effects. Staying well-hydrated supports all digestive processes. Medium-chain triglyceride (MCT) oil can be easier to digest for those with pancreatic insufficiency. Herbal remedies like ginger and peppermint may ease nausea, though they should never replace medical treatment.
Prevention Strategies: The most effective prevention methods involve lifestyle modifications. Limiting alcohol consumption or abstaining entirely significantly reduces pancreatitis risk. Quitting smoking is crucial, as it’s one of the most modifiable risk factors for pancreatic disease. Maintaining a healthy weight through balanced nutrition and regular exercise helps prevent metabolic stress on the pancreas. Managing conditions like diabetes, high cholesterol, and high triglycerides through medication and lifestyle changes protects pancreatic function. Regular health screenings are particularly important for those with family histories of pancreatic disease.

Health Tips for Pancreatic Wellness
Adopt a Pancreas-Friendly Diet: Focus on small, frequent meals rather than large portions to avoid overwhelming the pancreas. Emphasize lean proteins like chicken, fish, and legumes while limiting red and processed meats. Choose healthy fats in moderation from sources like avocados, nuts, and olive oil, while avoiding trans fats and excessive saturated fats. Reduce refined sugars and simple carbohydrates that spike blood sugar. Increase fiber intake through whole grains, vegetables, and fruits to support digestive health.
Stay Hydrated: Adequate water intake is essential for all digestive processes and helps the pancreas function optimally. Aim for at least eight glasses of water daily, and avoid excessive consumption of sugary beverages and caffeinated drinks that can strain the digestive system.
Exercise Regularly: Moderate physical activity for at least 30 minutes most days of the week helps maintain healthy weight, improves insulin sensitivity, and reduces inflammation throughout the body. Activities like walking, swimming, cycling, or yoga are excellent choices.
Monitor Your Medications: Certain medications can cause pancreatic inflammation as a side effect. Discuss all medications and supplements with your healthcare provider, and never stop prescribed medications without medical guidance.
Manage Stress: Chronic stress affects every bodily system, including digestion. Incorporate stress-reduction techniques such as meditation, deep breathing exercises, adequate sleep, and activities you enjoy into your daily routine.
Know Your Risk and Get Screened: If you have a family history of pancreatic disease, inform your doctor and discuss appropriate screening protocols. While there’s no routine screening for pancreatic cancer in average-risk individuals, those with strong family histories or genetic predispositions may benefit from specialized surveillance programs.
Listen to Your Body: Pay attention to persistent digestive symptoms, unexplained pain, or changes in your health. Early medical evaluation of concerning symptoms allows for prompt diagnosis and treatment, which significantly improves outcomes for pancreatic conditions.
By understanding these warning signs and taking proactive steps to protect your pancreatic health, you can reduce your risk of serious complications and maintain optimal digestive function throughout your life. Remember that persistent or severe symptoms should always be evaluated by a healthcare professional promptly.