Introduction
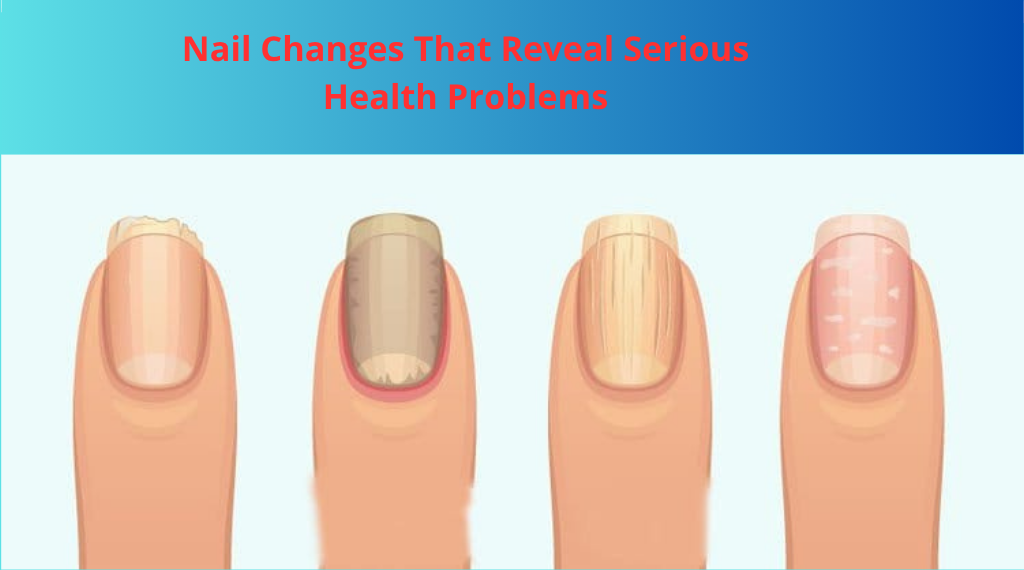
Your fingernails and toenails serve as more than just a canvas for polish—they function as windows into your overall health. These keratinized structures can reveal critical information about nutritional deficiencies, chronic diseases, infections, and systemic disorders long before other symptoms become apparent. Medical professionals often examine nails during physical assessments because changes in color, texture, shape, and growth patterns can indicate underlying health conditions ranging from minor deficiencies to life-threatening diseases. Understanding what your nails are telling you can lead to earlier diagnosis and treatment of serious health problems.
Causes and Risk Factors
Nail abnormalities arise from various physiological disruptions and disease processes:
Systemic Diseases: Conditions affecting multiple organ systems commonly manifest in nail changes. Cardiovascular disease can reduce blood flow to extremities, causing discoloration and changes in nail bed appearance. Kidney disease often results in half-and-half nails (Lindsay’s nails), where the proximal half appears white and the distal half reddish-brown. Liver cirrhosis may produce white nails (Terry’s nails), while diabetes increases susceptibility to fungal infections and slow healing.
Nutritional Deficiencies: Insufficient intake of essential nutrients directly impacts nail health. Iron deficiency anemia can cause spoon-shaped nails (koilonychia), while protein malnutrition leads to horizontal white bands (Muehrcke’s lines). Biotin, zinc, and vitamin B12 deficiencies also contribute to brittle, ridged, or discolored nails.
Infections: Fungal infections (onychomycosis) represent the most common infectious cause of nail abnormalities, causing thickening, discoloration, and crumbling. Bacterial infections, particularly involving Pseudomonas, can turn nails green, while viral infections like warts may affect the nail fold.
Medications and Toxins: Chemotherapy drugs frequently cause nail pigmentation changes, brittleness, and even nail loss. Antimalarial medications can produce blue-gray discoloration, while arsenic poisoning creates horizontal white lines (Mees’ lines).
Autoimmune Conditions: Psoriasis commonly affects nails with pitting, ridging, and separation from the nail bed. Lupus and other connective tissue diseases can cause nail fold inflammation, splinter hemorrhages, and clubbing.
Risk Factors: Advanced age, compromised immune function, poor circulation, repetitive trauma, prolonged moisture exposure, and genetic predisposition increase the likelihood of developing nail abnormalities that signal health problems.

Symptoms
Recognizing concerning nail changes requires attention to multiple characteristics:
Color Changes: Healthy nails appear pink with a whitish crescent at the base. Yellow nails may indicate fungal infection, respiratory disease, lymphatic problems, or diabetes. Blue or purple nails suggest oxygen deprivation from heart or lung disease. White nails can signal liver disease, anemia, or kidney problems. Dark streaks, particularly brown or black vertical bands (melanonychia), warrant immediate evaluation to rule out melanoma.
Texture and Shape Alterations: Clubbing—where fingertips enlarge and nails curve downward around them—indicates chronic low oxygen levels from lung disease, heart conditions, or inflammatory bowel disease. Spoon nails (koilonychia) that curve upward at the edges suggest iron deficiency. Horizontal ridges (Beau’s lines) indicate temporary growth disruption from severe illness, high fever, or chemotherapy. Vertical ridges typically represent normal aging but can occasionally indicate nutrient deficiency.
Separation and Lifting: When nails separate from the nail bed (onycholysis), it may indicate fungal infection, thyroid disease, psoriasis, or reaction to medications. This creates a whitish appearance and increases infection risk.
Pitting and Grooves: Small depressions or pits across the nail surface commonly accompany psoriasis but also occur with alopecia areata and other autoimmune conditions. Deep horizontal grooves suggest severe systemic stress.
Bleeding and Discoloration: Splinter hemorrhages—tiny blood clots appearing as dark red or brown vertical lines under the nail—can indicate endocarditis (heart valve infection), vasculitis, or trauma. Red lunulae (the crescents at nail bases) may signal heart failure, rheumatoid arthritis, or lupus.
Growth Abnormalities: Dramatically slowed growth or complete growth cessation indicates severe systemic illness. Unusually rapid growth can accompany hyperthyroidism or psoriasis.

Treatment and Prevention
Addressing nail changes requires treating underlying health conditions while providing supportive care:
Medical Treatments: The primary approach involves diagnosing and managing the root cause. This may include:
- Systemic disease management: Controlling diabetes, treating heart or lung conditions, managing kidney disease, and addressing liver problems
- Antifungal medications: Oral antifungals like terbinafine or itraconazole for fungal infections, often requiring several months of treatment
- Nutritional supplementation: Iron supplementation for anemia, biotin for brittle nails, protein supplements for malnutrition
- Topical treatments: Medicated nail lacquers, corticosteroid creams for inflammatory conditions
- Medication adjustment: Changing or discontinuing drugs causing nail toxicity when medically appropriate
- Surgical intervention: Partial or complete nail removal for severe infections, ingrown nails, or tumors
Natural and Supportive Remedies:

- Dietary optimization: Consuming adequate protein, iron-rich foods (lean meats, legumes, spinach), biotin sources (eggs, nuts, whole grains), and omega-3 fatty acids supports nail health
- Hydration: Adequate water intake maintains nail flexibility and prevents brittleness
- Moisturization: Regular application of moisturizers containing urea, lactic acid, or vitamin E improves nail and cuticle health
- Tea tree oil: Possesses antifungal properties that may help with mild fungal infections when applied topically
- Biotin supplementation: Studies suggest 2.5 mg daily may improve nail thickness and reduce splitting
- Gentle nail care: Keeping nails clean, dry, and properly trimmed prevents many problems
Prevention Strategies:
Preventing nail problems involves both general health maintenance and specific nail care practices. Regular health check-ups enable early detection of systemic diseases. Maintaining balanced nutrition ensures adequate vitamin and mineral intake. Protecting nails from trauma, harsh chemicals, and prolonged water exposure preserves nail integrity. Avoiding nail-biting and aggressive manicures prevents damage and infection. Wearing breathable footwear reduces moisture accumulation that promotes fungal growth.
Health Tips
Implement these practical strategies to maintain healthy nails and detect problems early:
Daily Nail Care: Examine your nails regularly for changes in color, shape, or texture. Keep nails clean and dry, as moisture promotes bacterial and fungal growth. Trim nails straight across to prevent ingrown nails, and file sharp edges smooth. Moisturize nails and cuticles daily, particularly after hand washing. Avoid cutting cuticles, which provide natural protection against infection.
Protective Measures: Wear gloves when cleaning with harsh chemicals or washing dishes for extended periods. Choose nail salons that sterilize instruments properly and never share nail clippers or files. Allow nails to “breathe” between polish applications, and use acetone-free removers when possible. Select shoes that fit properly and allow air circulation to prevent toenail problems.
Nutritional Support: Eat a balanced diet rich in lean proteins, dark leafy greens, nuts, seeds, eggs, and fish. Consider supplementation if dietary intake is insufficient, particularly biotin, iron, zinc, and omega-3 fatty acids. Stay well-hydrated by drinking adequate water throughout the day.
When to Seek Medical Attention: Consult a healthcare provider immediately if you notice sudden nail color changes, particularly dark streaks or bands; sudden nail clubbing or shape changes; persistent pain, swelling, or redness around nails; signs of infection including pus or increased warmth; nails separating from the nail bed; or any nail change accompanied by other symptoms like fatigue, shortness of breath, or swelling.
Lifestyle Modifications: Manage chronic conditions like diabetes and cardiovascular disease through medication compliance and lifestyle changes. Quit smoking, which impairs circulation to extremities and compromises nail health. Reduce stress through relaxation techniques, as severe stress can temporarily halt nail growth. Exercise regularly to improve circulation to hands and feet.
Professional Care: Schedule regular check-ups with your primary care physician, who can identify systemic causes of nail changes. See a dermatologist for persistent nail problems, suspected fungal infections, or concerning color changes. Consider podiatry care for chronic toenail issues, particularly if you have diabetes or circulation problems.
By paying attention to your nails and understanding what changes might signify, you become an active participant in monitoring your health. While not every nail change indicates serious disease, recognizing patterns and seeking timely medical evaluation can lead to earlier diagnosis and better outcomes for underlying health conditions.